
Multidisciplinary teams (MDT)
Multidisciplinary team-based models of care
What is a multidisciplinary team (MDT)?
A multidisciplinary team (MDT) in a general practice setting involves healthcare professionals such as GPs, nurses, pharmacists and other allied health professionals, and specialists working together to deliver coordinated care for patients. Each team member contributes their expertise to enhance patient outcomes, reduce hospital admissions, and ensure comprehensive management of chronic conditions (see Figure 1).
How is multidisciplinary team (MDT) care delivered in general practice?
Across our region, practices are using a variety of flexible models to support multidisciplinary care, often combining several arrangements to meet local needs. The most common approach involves directly employing nurses and occasionally allied health professionals, funded in part through the Workforce Incentive Program – Practice Stream (WIP-PS), allowing them to play a central role in care coordination.
Others engage health professionals as contractors for specific services or utilise consulting room rental agreements to bring services onsite without assuming employment responsibilities.
Some practices share staff across multiple sites to sustain part-time roles or establish preferred referral pathways with nearby providers to expand patient access.
In more complex cases, such as chronic pain or mental health, referrals may be made to specialised interdisciplinary teams, though these are less common.
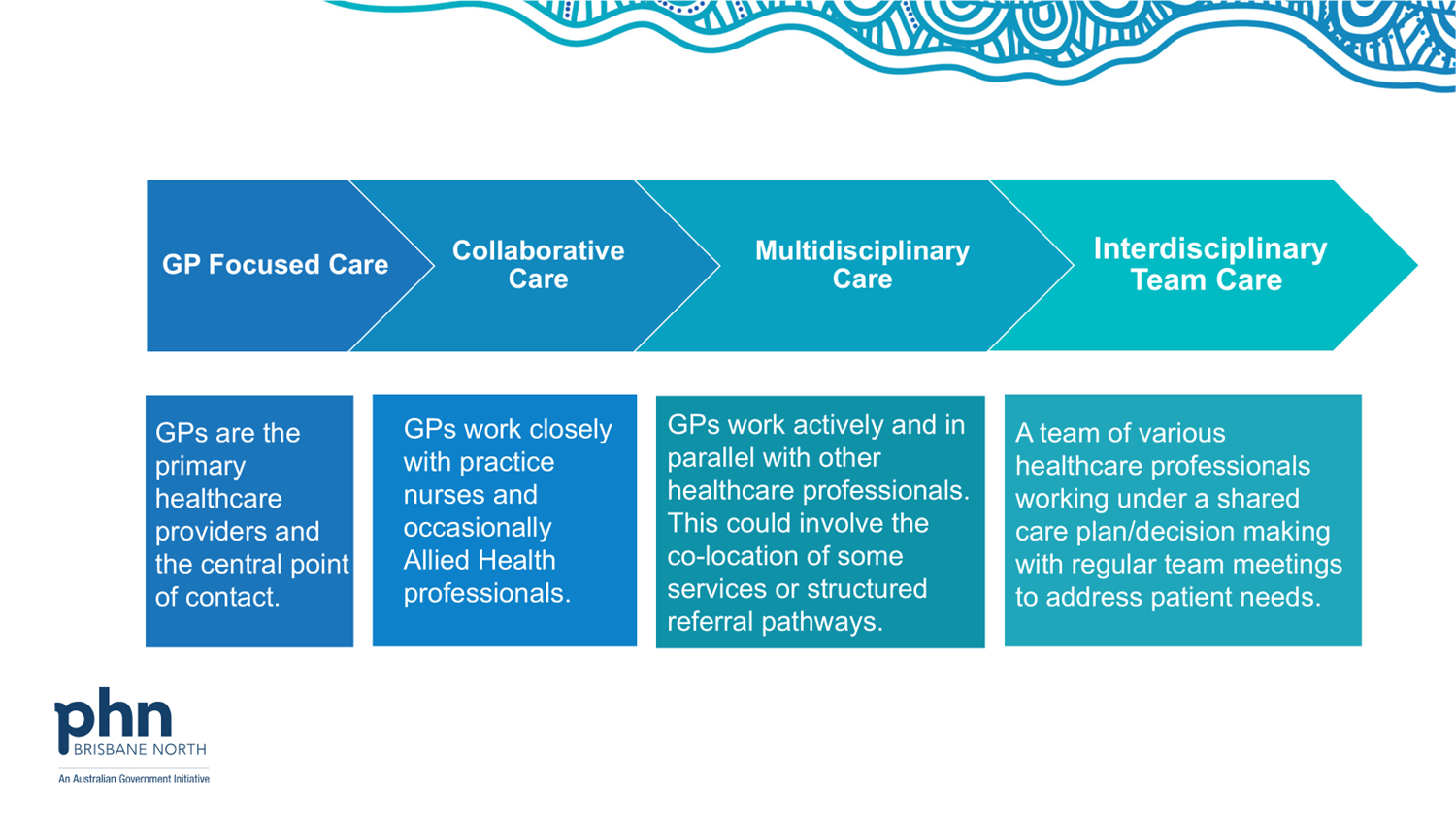
Each model varies in its level of integration, governance, and sustainability, but collectively they illustrate the growing adaptability and commitment of practices to delivering team-based, patient-centred care. A continuum of integration, from solo GP care through to fully coordinated, team-based service delivery, is illustrated in Figure 1 showcasing an increasing collaboration between GPs and non-GP healthcare professionals as moving towards multidisciplinary care.
Multidisciplinary team (MDT) integration spectrum
Figure 1 (above)
This continuum illustrates the varying levels of integration in primary care models, based on the degree of collaboration between general practitioners (GPs) and non-GP health professionals. It provides a useful framework for understanding how care models range from GP-focused to fully interdisciplinary, team-based care. The framework highlights how practices may evolve their approach to better meet the needs of patients with increasing complexity through improved coordination, communication, and shared care planning.
De-identified case studies: how teams work together
Explore case studies which champion real-life examples of multidisciplinary models of care from across our region:
- case study from a large, interdisciplinary practice
- case study from a community-controlled health organisation
- case study from a GP practice group with a chronic disease focus.
Practice Ownership and Business Management

